Hmm … it looks like your browser is out of date.
Let’s update your browser so you can enjoy a faster, more secure site experience.
2026 UHC Dual Complete WY-S001 (PPO D-SNP)
Medicare
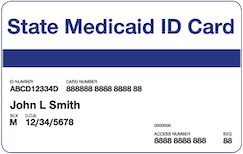
What is a dual special needs plan?
H2001-049 -000
Monthly premium: $0.00 *
*Your costs may be as low as $0, depending on your level of Extra Help.
This Preferred Provider Organization (PPO) plan gives you more benefits than Original Medicare, all with as low as a $0 plan premium. You'll keep all your Medicaid benefits, and add even more. Must have full Medicaid benefits, or be a Qualified Medicare Beneficiary (QMB) with all your Medicare-covered services provided at $0: WY: FBDE, QMB, QMB PLUS, SLMB PLUS
- 2026 UHC Dual Complete WY-S001 (PPO D-SNP)
1-844-812-5967 TTY: 711 8 a.m.-8 p.m. local time, 7 days a week
Find providers and coverage for this plan.
Search for doctors, hospitals, and specialists.
Search for providers, clinics and treatment centers.
Find medications covered by this plan.
Find a dentist near you.
Find a pharmacy near you.
Benefits & features
$0 copay for network dental like exams, x-rays, routine cleanings and fluoride
$81 credit every month for OTC, plus healthy food and utilities for qualifying members
$150 allowance for eyewear every year, plus $0 copay for a routine eye exam and lenses
$1,500 allowance for a broad selection of OTC and brand-name hearing aids
Free gym membership at core and premium locations
Routine foot care
4 foot care visits for nail trims and other covered preventive care
No cost medical services
$0 copay for primary care, hospital stays and specialist visits
Prescription drug coverage
$0 copay for Tier 1 prescriptions
Provider network
See any provider in our large provider network
Optum HouseCalls
Yearly in-home visit to help support your health
Benefits, features and/or devices may vary by plan/area.
Limitations, exclusions and/or network restrictions may apply.
OTC, food and utility benefits have expiration timeframes.
Review your Evidence of Coverage (EOC) for more information.
The healthy food and utilities benefit is a special supplemental benefit only available to chronically ill enrollees with a qualifying condition, such as diabetes, cardiovascular disorders, chronic heart failure, chronic high blood pressure and/or chronic high cholesterol, and who also meet all applicable plan coverage criteria. There may be other qualified chronic conditions not listed.
If your plan offers out-of-network dental coverage and you see an out-of-network dentist, you might be billed more. Network size varies by local market.
Review your plan Drug List (Formulary) on UHC.com/Medicare for a list of covered prescription drugs, including those on Tier 1.
Annual routine eye exam and an allowance for contacts or one pair of frames, with standard (single, bi-focal, tri-focal or standard progressive) lenses covered in full every year. Review your Evidence of Coverage (EOC) for more information.
The plan only covers hearing aids from a UnitedHealthcare Hearing network provider. Other hearing exam providers are available in the UnitedHealthcare network.
The fitness benefit and gym network varies by plan/area and participating locations may change. The fitness benefit includes a standard fitness membership at participating locations. Not all plans offer access to premium locations. Consult your doctor prior to beginning an exercise program or making changes to your lifestyle or health care routine.
Network size varies by local market and exclusions may apply.
Referrals may be needed to see network specialists.
Optum HouseCalls may not be available in all areas.
UHC Dual Complete WY-S001 (PPO D-SNP)
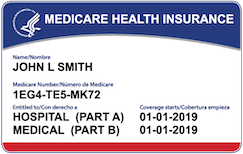
Monthly plan premium for people who get Extra Help from Medicare to help pay for their prescription drug costs
If you get Extra Help from Medicare to help pay for your Medicare prescription drug plan costs, your monthly plan premium will be lower than what it would be if you did not get Extra Help from Medicare. The amount of Extra Help you get will determine your total monthly plan premium as a member of our Plan.
This table shows you what your monthly plan premium will be if you get Extra Help.
| Your level of Extra Help | Monthly premium* |
|---|---|
| 100% | $0.00 |
*This does not include any Medicare Part B premium you may have to pay.
If you aren’t getting Extra Help, you can see if you qualify by calling:
- 1-800-Medicare or TTY users call 1-877-486-2048 (24 hours a day/7 days a week),
- Your State Medicaid Office, or
- The Social Security Administration at 1-800-772-1213. TTY users should call 1-800-325-0778 between 7 a.m. and 7 p.m., Monday through Friday.
Your health care needs are unique. These documents can help you make sure you get the right coverage.
Documents include Annual Notice of Changes, Evidence of Coverage, Formularies, Medicare Plan Star Ratings, Provider Directories, Summary of Benefits, Other downloadable resources.
Learn more about dual special needs plans
Learn more
UHC Dual Complete WY-S001 (PPO D-SNP)